19% of Patients with a Medicare-Reimbursed Off the Shelf Device Later Receive a Custom Device

New analysis from Dobson DaVanzo: 19% of patients with a Medicare-reimbursed Off the Shelf device later receive a custom-fitted or custom-fabricated orthotic device
Medicare’s own data shows that frequently patients who receive a Medicare-reimbursed OTS device subsequently also receive a Medicare-reimbursed custom-fitted or custom-fabricated orthotic device. Clearly, some modest portion of these data reflect instances in which OTS devices are fitted out of necessity in the acute or emergent setting and occasionally with the knowledge that a custom-fitted or custom-fabricated orthotic device will be required further down the road. There are also instances with progressive disorders where an OTS device may be sufficient for a period of time before their condition warrants a custom-fitted or custom-fabricated orthotic device. Clinical experience indicates that such instances could account for a relatively small portion of the 19%. But it also appears likely that there is a very significant percentage of cases where OTS devices do not fully or appropriately meet the patients’ needs.
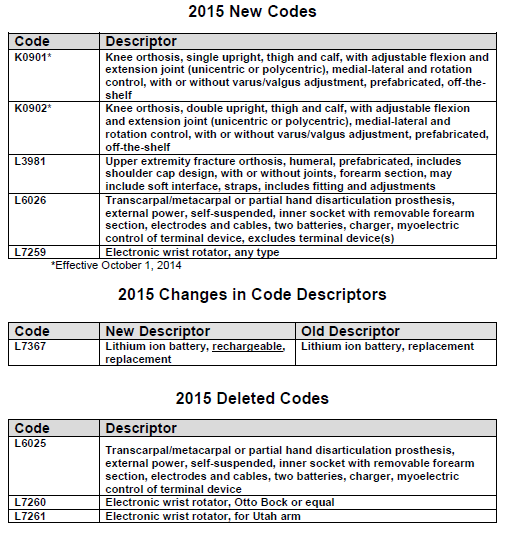
| Type | Total Patients | RECEIVED OTS AS FIRST ORTHOTIC DEVICE | SUBSEQUENTLY RECEIVED CUSTOM FITTED/FABRICATED DEVICE | ||
|---|---|---|---|---|---|
| Patients | Percent of Total Patients | Patients | Percent of OTS Patients | ||
| TLSOs | 20,408 | 1,519 | 7.4% | 163 | 10.7% |
| LSOs | 197,906 | 19,917 | 10.1% | 3,372 | 16.9% |
| AFOs | 268,232 | 56,959 | 21.2% | 11,359 | 19.9% |
| Total | 486,546 | 78,395 | 16.1% | 14,894 | 19.0% |
Source: Dobson-DaVanzo analysis of custom cohort Standard Analytic Files (2007-2010) for Medicare beneficiaries who received O&P services from January 1, 2008 through December 31, 2008.
It appears that delivering substantial numbers of OTS devices without any accompanying adjustment and clinical care may not result in patients getting better, but results, at least in a substantial number of instances, in wasted Medicare funds on that OTS device AND a delay in the patient receiving any improvement in their symptoms/ health. In this unfortunate reality, both the patient and the Medicare program will be negatively impacted as a result of increase patient co-payments and additional expenses to the Medicare program, and a disregard for patient health for Medicare beneficiaries as a result of CMS mandating that devices be provided to patients without professional adjustment and fitting, contrary to the premises for FDA-approved labeling.